What do we know about Covid-19 inequalities among people from minority ethnic groups?
In the early stages of the coronavirus epidemic in the UK, and in the absence of data splitting out Covid-19 deaths by ethnicity, reports of health workers from minority ethnicities dying of Covid-19 was the first clue that some groups of people might be disproportionately affected by the disease.
Following calls for more consideration to be given to the issue, on 16 April the government announced it would launch a review into the impact of Covid-19 on different ethnic groups.
The review by Public Health England (PHE) was published on 2 June, and found that people from minority ethnic groups are more likely to get severely ill and die from Covid-19 compared to the majority White population in the UK.
Similar inequalities have also been reported in other countries including the USA and Norway.
Emerging evidence has begun to piece together the different factors that help to explain why Covid-19 affects people from some ethnic groups more than others.
This includes factors that make catching Covid-19 more likely, such as overrepresentation in key worker roles, living in crowded housing and urban areas, and factors that make a severe illness more likely, such as underlying health conditions.
It is difficult to separate out the precise impact of each of these risk factors on Covid-19 outcomes. Further, even after taking these factors into account, some of the inequality between people of different ethnicities remains.
This article presents what is known and, perhaps more importantly, unknown about inequalities in Covid-19 outcomes across minority ethnic groups in the UK.
Join 72,547 people who trust us to check the facts
Subscribe to get weekly updates on politics, immigration, health and more.
Rates of severe Covid-19 infections and deaths differ by ethnic group
Many studies show that people from minority ethnic groups are more likely to have a severe Covid-19 infection compared to White ethnic groups (including White British and other White ethnicities) in the UK. That is not in dispute.
However, the extent of reported inequality differs across the research and so it can be difficult to build a coherent picture about any aspect of this new illness. This is particularly the case for ethnicity and Covid-19 where studies vary in key ways. Depending on how each study was done, the results can tell you different things and that should be kept in mind when looking at the data.
For example, different studies look at different outcomes, from people testing positive for the coronavirus that causes Covid-19, SARS-CoV-2, to the most severe Covid-19 cases, which require hospitalisation or lead to death.
Some studies may look at differences in outcomes between ethnicities across the whole population. While others may focus exclusively on people who become hospitalised with Covid-19. These tell us about outcomes once in hospital, but do not tell us anything about the likelihood of ending up in hospital in the first place.
Another prominent reason for differences is the number of other risk factors for Covid-19 illness, asides from ethnicity, that are included (“adjusted for”) in analyses. Adjusting for risk factors means that variation in those factors between groups is taken out of the reported risk of severe Covid-19 illness.
For example, sex and age are commonly standardised in health research to produce more comparable results between different groups. Accounting for age is particularly important here as people from ethnic minorities, on the whole, are much younger than the wider population. Not taking age into account means we could miss some of the increased risk of severe illness among minority ethnic groups.
It is important to note where additional risk factors, for example socioeconomic circumstances and health conditions, are also included in analyses. Adjusting for factors that help to explain different Covid-19 outcomes by ethnic groups (known as mediators) may be introducing overadjustment bias into study results. This can mean that the final reported risk of illness does not capture the full picture of inequality experienced by different groups.
There are ways to look at the individual contribution of mediators in research, but we have seen few Covid-19 studies that use these methods so far. The majority of studies below present adjusted results. This doesn’t mean they are not useful, but there may be alternative methods that could be used to more precisely measure the contribution of different risk factors to inequalities.
So what do the statistics show us?
PHE found that Black people are two to three times more likely to have been diagnosed with Covid-19 compared to White people, after adjusting for age. This covered the period to 9 May, when testing was not widely available outside hospitals, and so testing positive usually indicated a serious illness.
Intensive care audit data, up to the 14 May 2020 found that people from minority ethnicities made up 33% of Covid-19 cases treated in critical care (compared to 13% of the general UK population at the 2011 censuses). A study of people admitted to hospital with Covid-19 across Great Britain found that, compared to White people, Black people were 36% more likely and South Asians 28% more likely to be admitted to a critical care facility, after adjustment for age, sex and location.
Fifty-six percent of pregnant women admitted to hospital in the UK from 1 March to 14 April 2020 with SARS-CoV-2 were from a minority ethnic group, a study has found. Compared to White pregnant women, this study estimates that Black women were over eight times more likely and Asian women four times more likely to be admitted to hospital with SARS-CoV-2.
Additionally, informal reports of children with a Covid-19 linked inflammatory syndrome from the UK suggest rates of this condition are higher in minority ethnic groups, particularly those from a Black ethnicity.
As with serious illness, people from minority ethnic groups are also more likely to die of Covid-19 than White people.
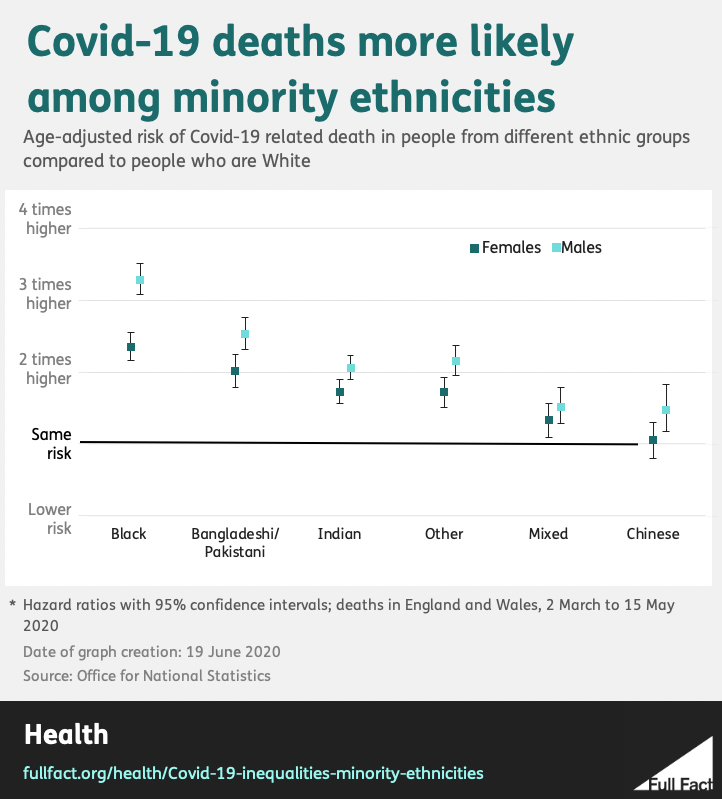
To look at Covid-19 related deaths by ethnic group, the Office for National Statistics (ONS) linked death registrations in England and Wales to 2011 Census data. This data only includes people living in private households at the 2011 Census.
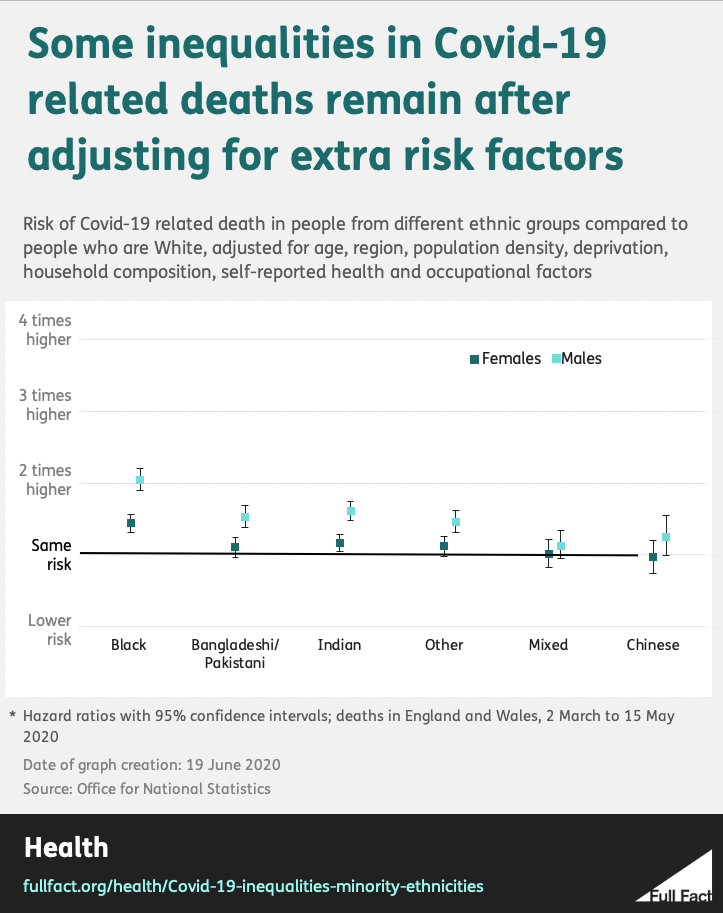
As shown below, after adjustment for age, the ONS found an increased risk of death across all ethnicities (apart from Chinese women) when compared to White groups. After adjustment for occupational risk and various other regional, social and economic factors, the increased risk for people from minority ethnicities got smaller, and disappeared for some, but not all.
PHE have looked at Covid-19 related deaths among people who had a positive SARS-CoV-2 test result. It found that people of Bangladeshi ethnicity had about twice the risk of death compared to White British people, after adjustment for sex, age, deprivation and region. After adjustment, the report found that “people of Chinese, Indian, Pakistani, Other Asian, Caribbean and Other Black ethnicity had between 10 and 50% higher risk of death when compared to White British”.
Why do we see these patterns?
As mentioned, when trying to explain this disproportionate effect, there are two things to consider: why people from minority ethnicities might have a higher risk of being exposed to the disease in the first place and, after contracting the virus, have a higher risk of a severe Covid-19 illness.
We can’t use the current evidence, based on people with a severe Covid-19 illness, to work out exactly how much of Covid-19 inequalities are due to each, because we simply don’t know the rates of infection among people from minority ethnicities.
A greater proportion of people from minority ethnicities have tested positive for Covid-19 than White people, after adjusting for age and sex. But this data can’t be used to look at whether people from minority ethnicities are more likely to have been infected, because testing hasn’t been comprehensive.
Large-scale infection and antibody studies may help to work this out. A survey run by the ONS that tries to measure the true incidence of Covid-19 in the population by randomly testing people, regardless of symptoms, doesn’t split out its data by ethnicity.
What we can do is look at some of the possible factors that could increase the risk of infection and illness for people from minority ethnicities (many of which are captured in the adjusted data presented above). While some risk factors are specific to increased infection risk or an increased risk of severe illness, some of these risk factors apply to both.
Risk of infection
Some minority ethnic groups might be more exposed to the virus as they are more likely to work in essential key worker roles—meaning that they continued to work outside their home through the coronavirus outbreak. Using data from the UK Labour Force Survey, the IFS Deaton Review into inequalities found that “Pakistanis, black Africans and black Caribbeans are over-represented among key workers overall”.
These groups are particularly likely to work in health and social care roles: occupations that are at particular risk of coming into contact with contagious people. According to the IFS’s analysis, people from a Black African ethnicity account for 7% of nurses (compared to 2.2% of the working-age population) and people from an Indian ethnicity make up 14% of doctors (compared to 3.2% of the working-age population).
Spread of the new coronavirus in the UK has been more rapid in cities, where people from minority ethnicities are more likely to live. This is reflected in ONS mortality data, which shows that the rate of Covid-19 related deaths registered in England and Wales between 1 March 2020 and 17 April 2020 (after adjustment for age) was at least three times greater in major urban areas compared to rural towns. Factors such as the large flows of visitors from other countries, reliance on public transport and, to a lesser extent, population density have been proposed to explain this association.
Higher rates of Covid-19 infections and deaths have been seen in areas with higher deprivation; areas where people from minority ethnicities are also more likely to live.
The precise reasons for this association are yet to be determined, but in conjunction with factors related to living in an urban area, it is thought that employment in low paid essential jobs and living in crowded housing and multigenerational households (more likely among minority ethnic groups) play a role.
In these circumstances, social distancing is more challenging and viral transmission therefore more likely.
Risk of severe illness
The ONS analysis shown above suggests that occupational, geographical and socioeconomic factors explain a substantial proportion of the excess risk of death from Covid-19 among minority ethnic groups. However, beyond pointing to increased exposure to SARS-CoV-2, this doesn’t tell us how these factors lead to worse outcomes.
Based on what is known about other respiratory conditions, vulnerability to severe illness is likely to be increased through a combination of factors including smoking, poor housing conditions, inadequate nutritional intake and pre-existing physical and mental health problems.
Access to green spaces and exposure to pollution are also said to be a key determinant of health inequalities. Early evidence suggests that higher levels of ambient air pollution (from traffic and industrial sources, for example) are associated with higher rates of Covid-19 deaths.
Experience of some of these factors is more common among people from minority ethnicities (such as living in areas with high air pollution) while some are less common (such as smoking).
Health conditions known to put people at greater risk for severe Covid-19 illness, including diabetes, heart conditions, kidney disease and obesity, are more prevalent in some minority ethnic groups. Data compiled by the IFS shows that, in people over the age of 45, long term “at-risk” health problems are almost twice as prevalent in Bangladeshi groups, and about 1.2 to 1.4 times more prevalent in Pakistani, Indian and Black African groups compared to White British groups.
Underlying health conditions are not currently included in analyses by PHE and only self-reported measures of health in ONS analyses. However, these conditions are more prevalent among people living in poor socioeconomic circumstances, something that is included in their analyses. This means that some of the risk of getting a severe Covid-19 illness caused by underlying conditions will be captured by other risk factors included in the analyses.
A study covering 260 hospitals in Great Britain found that South Asian people had a 19% increased risk of death once admitted to hospital for Covid-19 than White people. Using methods to look specifically at mediators, this study found that about 18% of this increased risk was explained by diabetes.
Differences in health seeking behaviour (meaning the actions taken when someone believes they are ill) have been proposed as a contributing factor to Covid-19 inequalities. However, a study of hospital admissions found no difference in the duration or severity of Covid-19 symptoms by ethnicity when patients were admitted to hospital. This suggests that people from different ethnic groups with severe Covid-19 are seeking help at about the same time in their illness, so health seeking behaviour is unlikely to contribute to different outcomes once patients are in hospital at least.
There are other factors that may specifically affect people who have migrated to the UK, regardless of ethnicity. For example migrants may be more likely to avoid accessing healthcare altogether because of confusion over NHS charges. The UCL–Lancet Commission on Migration and Health writes that “whilst migrants diagnosed with COVID-19 are exempt from healthcare charges, not all migrants will be aware of these exemptions and the exemption first requires a diagnosis.”
There are still many unknowns
Even where research has accounted for geography, socioeconomic circumstances and clinical factors, the association between Covid-19 outcomes and ethnicity persists.
It has been suggested that biological and genetic factors may partially explain the differences between ethnic groups. Differences in immune responses and in enzyme receptors that regulate how viruses are able to infect the body have been proposed as explanations, but there is currently a lack of evidence specifically relating to Covid-19 outcomes to back up these theories.
Vitamin D deficiency, which is more common in minority ethnic groups, has also been suggested as a reason for the increased risk. However, the evidence for this is mixed with a UK Biobank study concluding that vitamin D concentration does not explain differences in Covid-19 infection between ethnicities.
Looking at biological and genetic links poses more questions about how we define ethnicities.
An ethnic group (or ethnicity) is defined as “the social group a person belongs to, and either identifies with or is identified with by others, as a result of a mix of cultural and other factors including language, diet, religion, ancestry, and physical features”.
The genes that are responsible for observable physical features are few, and genetic differences within people of the same ethnicity are greater than those between different groups.
Statistics produced by the UK government tend to use broad categories to group ethnicities. This classification system, as explained by the Scottish Health Observatory, represents a pragmatic approach to “identify variations that are important for research and policy”.
However, it is argued that analysis of Covid-19 inequalities should look at subgroups (beyond broad categories) to better understand the complex factors that bring about these health differences.
All of these factors are impacted by other inequalities too
Finally, it’s worth noting that observing that some people from minority ethnicities suffer poorer health outcomes is far from a new phenomena and not specific to Covid-19.
Looking at what is already known from research on other health conditions can help us understand inequalities in Covid-19 outcomes.
In a report on understanding and reducing ethnic inequalities in health, PHE says: “Racist discrimination impacts indirectly to produce poorer health outcomes via exclusionary processes operating within the education system and within the employment and housing markets.
“These processes result in differential access to health-promoting resources and exposure to health-damaging risks.”
As mentioned, migrants may be less likely to access healthcare in general which could lead to worse outcomes.
Evidence from the health and social care sector also illustrates the barriers faced by minority ethnic groups. The Kings Fund lists several ways discrimination is experienced by minority ethnic NHS workers, from bullying and harrassment from other staff members and patients, to lower pay, less chance of promotion and underrepresentation in senior positions compared to White peers.
These experiences may influence Covid-19 outcomes both indirectly, through their influence on socioeconomic circumstances and health issues, and directly, through increased exposure through frontline roles and reduced access to Personal Protective Equipment (PPE).
In summary, people from minority ethnic groups do have higher risks from Covid-19 than the majority White population in the UK. We don’t know the extent to which this is due to a higher risk of infection and the extent to which this is due to a higher risk once infected.
However, the evidence presented above suggests both play a part.
There also appears to be additional risk for people from a minority ethnic background, which is not explained by socioeconomic and geographical factors associated with being from these groups. The precise components that contribute to this additional risk are unknown at present, but are likely to largely stem from the wider social experience of being a minority.
Correction 3 July 2020
We corrected an error in this article which stated that people of Bangladeshi ethnicity had about 200% greater risk of death, among confirmed Covid-19 cases, compared to White British people after adjustment for sex, age, deprivation and region. We also corrected an error which wrongly stated the date on which the graphs were produced.