The claim is about 700 extra transplants happening a year. That could save or improve the lives of 700 people, who may or may not otherwise have died in the same year.
700 extra transplants a year is based on improving family consent rates for organ donation to “world class” levels. Whether or not the claim is correct rests on whether the government’s policy package will help increase consent rates at all or by enough, and how accurately the effect of increased consent on the number of transplants is being calculated.
As the government itself admits, there is limited evidence for how much its plans will deliver improved consent rates for organ transplants, if at all. It’s plausible the system could reduce consent rates as well, but again the evidence for this in the context of the planned changes in England is limited.
The modelling behind the claim—converting an increased consent rate into the number of extra transplants—also rests on a lot of assumptions.
All in all, this claim hinges precariously on a lot of uncertainty.
Some people in the UK choose to allow their organs to be donated after they die. Others donate while they’re still alive—people can survive with one kidney, for example.
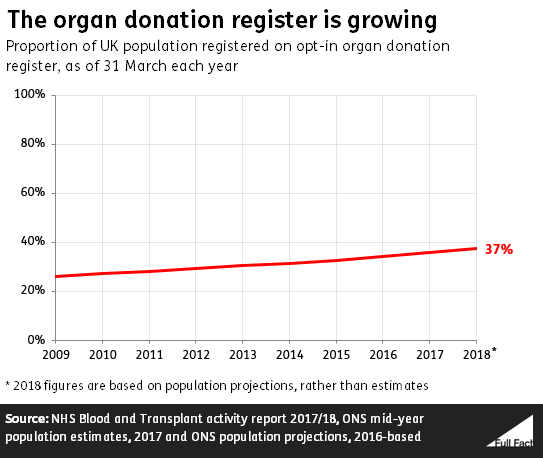
There are just under 25 million people on the NHS opt-in organ donation register in the UK—about 37% of the population.
As we’ll explain more later, this doesn’t automatically mean they’ll end up being donors, nor does it mean that people who aren’t on the register won’t have their organs donated after death. About half of deceased organ donors last year were on the donor register.
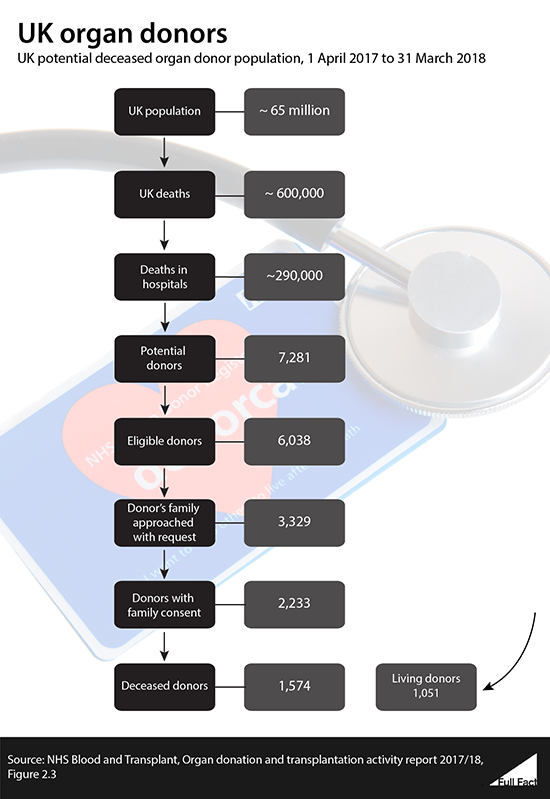
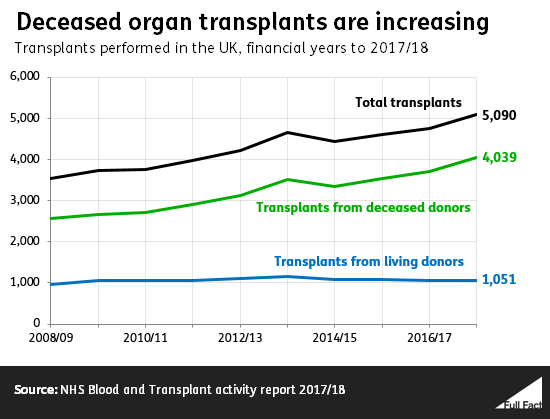
Last year only about 1,600 deceased people actually became donors, the drop-off mainly due to further medical concerns, logistical hurdles, or not getting consent from their families. People can donate more than one organ, and last year around 4,000 transplants took place from deceased donors.
Donations after death are more common than living donations, but they’re still relatively rare because they can only happen when people die in certain circumstances, and are medically suitable for a donation.
So when the government talks about saving 700 more lives a year, they’re talking about increasing the number of transplants above 4,000.
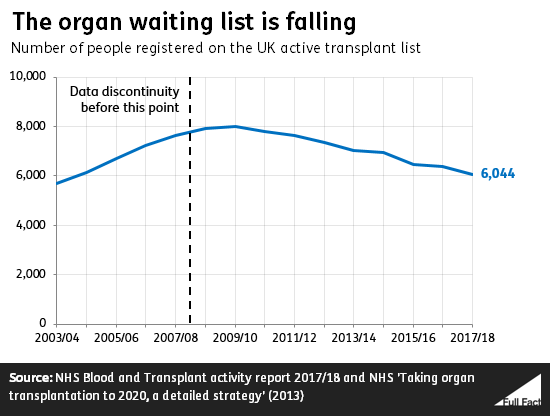
There is a shortage of organs available for transplant in the UK and some people still die waiting for a transplant. We don’t know exactly how many people die every year as a result of not getting a needed organ transplant, as there isn’t complete data.
In 2017/18, 411 people died while waiting on the transplant list, and a further 755 were removed from the transplant list, mostly because they had become too ill. Many of those patients would have died shortly afterwards, but we don’t know about their circumstances after leaving the list.
Meanwhile around 6,000 people are currently waiting for an organ in the UK.
How organ donation currently works in the UK
At the moment, the system for organ transplants is different in different parts of the UK, because the health system is devolved.
In England, doctors need to get consent before they can remove organs from someone for a transplant. They aren’t allowed to do so if the deceased person had previously refused consent. If no view had been expressed either way, consent is sought from an eligible relative.
They are allowed to proceed if the deceased had given consent, but they’re still not obliged to do so, for example if the deceased’s relatives object.
The system is similar in Scotland and Northern Ireland.
Wales changed to an opt-out system in 2015. Here, consent is assumed from adults unless they have registered their wish not to be a donor. There are still restrictions on when doctors can proceed with a transplant, and relatives of the deceased can still stop the procedure.
The UK government wants to introduce a similar system in England, which is what’s behind the news this month.
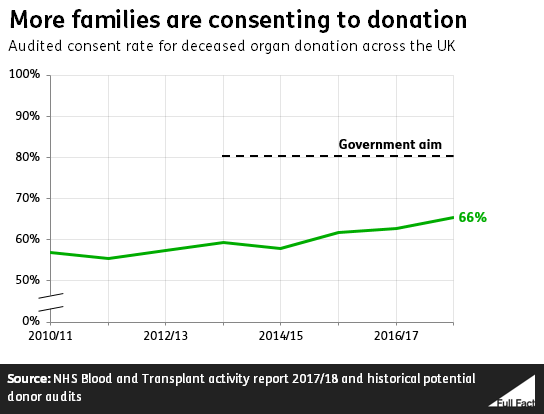
The current UK ‘consent rate’ for organ donation is around 66%
There are a lot of barriers to an organ transplant taking place. The most significant ones are based on whether the patient was on ventilation before death, and whether the patient’s medical condition is suitable. Only if those tests are passed is consent sought from relatives of the deceased.
A key measure of consent is called the ‘consent rate’, which looks at how many cases involved the family being approached and of these, how often consent was given.
In 2017/18, across the UK, consent was given an estimated 66% of the time when families were asked. Even then, only 70% of these cases where consent was given resulted in an actual donation last year.
Families don’t give consent for a variety of reasons. The most common include the patient having previously expressed a wish not to donate, when the family aren’t sure what the patient’s wishes would have been, the family feeling the process would take too long, and not wanting surgery done to the body.
The consent rate is the baseline from which the effects of policy changes—and so how many extra people’s lives might be saved—are calculated.
The Department of Health and Social Care, in conjunction with NHS Blood and Transplant, uses a model to work out how changes to the consent rate might change the number of donors. This involves making a lot of assumptions, and isn’t a perfect predictor of what would actually happen.
The government uses the consent rate from 2016/17—63%—as its baseline. If that 63% could be increased to 80%—the government’s ambition—this model suggests that could mean around 700 extra transplants every year.
The actual impact assessment doesn’t mention the 700 figure, its central estimate is a much lower increase to a consent rate of 70%—resulting in around 250 extra transplants. Our calculations suggest 700 is roughly what the model would show if rates increased to 80%.
NHS Blood and Transplant told us the estimates that were actually published in the impact assessment weren’t predictions, they were just examples of what the model would show. They explained this was because the evidence was so uncertain.
In an early draft of the impact assessment behind the policy, the Department for Health and Social Care said:
“The Government proposes to set an ambition to see consent rates increased to 80%. If this can be realised, it would mean about 280 more donors than current levels, which is equivalent to about 700 more organ transplants.”
A key assumption to all of these estimates is that the number of people who are medically suitable to donate organs doesn’t change in future years.
There is no clear evidence the government’s plans will increase consent rates, or by how much
In summarising its impact assessment, the government says immediately that the evidence behind the policy is scarce:
“Would opt-out change the organ donation consent rate? The evidence is inconclusive.
“While it seems that moving to an opt-out system is unlikely to decrease the consent rate, there is no unambiguous evidence that opt-out by itself increases consent rates.
“There is evidence that in some cases, when opt-out is implemented alongside other pro-organ donation policies, such as communications campaigns, consent rates increase.”
This last point reflects the conclusion of the government’s Chief Scientific Adviser, who looked at the available evidence and said “with moderate certainty”, that when introduced as part of a wider communication and logistical package, opt-out systems can be associated with higher donation rates.
The government plans to do a communications campaign alongside the change in the policy anyway, so it thinks that the overall effect will be some positive shift in rates.
Could consent rates actually fall with the policy change?
Plausibly. The conclusions of the government’s Chief Scientific Adviser leave some room for doubt.
The reasoning behind this possibility comes down to the fact that under both the existing system in England and the proposed new one, the family of potential donors still have an effective veto in some situations, especially where there’s uncertainty as to the deceased person’s wishes.
One theory is that families may be more likely to withold consent under a presumed consent system than under the current opt-in system.
As one recent study for Queen Mary University London found, consent rates can be lower in ‘opt-out’ systems because there is less of a clear signal of a deceased person’s wishes. In an opt-in system, people give a clear indication that they wish to donate. As the study said: “in the event of uncertainty, families are more likely to refuse consent”.
However it also cautioned that ‘opt-out’ alone wasn’t necessarily a bad policy, it’s just usually associated with creating more uncertainty. It said an effective system depends on people being well-informed about what the consent system is, on families talking to each other about their wishes, and on people having the ability to register their preferences clearly, to reduce uncertainty.
This study alone can’t be used to prove the planned changes in England will reduce consent rates. For one thing, the government plans to keep the Organ Donation Register, so there will still be a route for people to express their wishes in this way.
But the research, along with the government’s own impact assessment, does show there’s a live debate as to whether the ‘opt out’ element of the organ transplant system actually makes consent more likely, or if it actually makes families more likely to refuse consent.
There are other ways of increasing the organ donation rate that may be more effective
Increased consent rates don’t go hand-in-hand with more transplants. The transplant system has to be able to cope with an increased caseload.
As part of its impact assessment the government admitted that the transplantation system is currently under “considerable pressure” and that without increased investment in capacity, increased consent rates wouldn’t necessarily see a corresponding increase in more transplants. For that reason, its policy plans also allow for the possibility of increased investment in the system itself, alongside the other costs.
How well the system runs is also a factor.
Spain has one of the most consistently high rates of organ donation in the world. In 2016, its organ donation rate (the number of deceased people that become donors) was 43.4 per million people, compared with 21.1 in the UK, and its consent rate was about 85%.
When Wales was considering introducing an opt-out system, an Assembly Committee visited Spain to see why organ donation rates were so high there. It concluded that improvements to the Spanish system were mainly the result of “good organisation”.
More important than changes to the consent system and publicity campaigns, it felt, were organising services to ensure that more potential donors become actual donors. This means things like training more medical staff to coordinate transplants and better national coordination of donors and recipients.
In the UK, one factor that is already associated with higher consent rates from families is the presence of a specialist nurse when the family is approached. These nurses provide support to families during the consent process, and are currently present in nine out of ten cases where families are approached.
Jackie Doyle-Price MP has said that “the system that we are looking to introduce has much in common with that in Spain”: meaning that changes to the consent system are only one aspect of what the Government has planned for the organ donation system in England.